SC Home Health is a not-for-profit affiliate of Springfield Clinic
Home health is a program of care and support for individuals recovering from illness, injury, new diagnoses, changes to medications, recent surgery or hospitalization. The focus is on recovery, rehabilitation and health education.
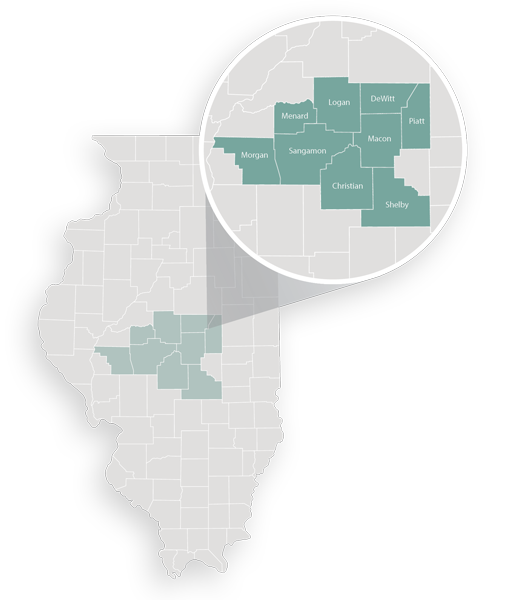
Our team provides care for patients residing in the following counties:
Champaign
Christian
DeWitt
Logan
Macon
Menard
Morgan
Piatt
Sangamon
Shelby
Contact Us
Phone: 217.462.0355
Fax: 217.462.0356
Email: [email protected]

